Penicillin Allergy: A Label That Can Affect Your Health
Betty Chaffee/ February 2, 2023/ Allergy, Medication Management/ 0 comments
It's likely that many of you who are reading this post have a penicillin allergy written in your medical record. As a matter of fact, about one in ten patients in the US report having a penicillin allergy. In my own experience as a pharmacist, I've seen penicillin listed as an allergy more often than any other medication.
The interesting thing is that when it's tested, nearly everyone who reports a penicillin allergy is actually not allergic to it! There are a number of reasons for that. One is that people often outgrow penicillin allergies. Up to 80% of people with a severe penicillin allergy will no longer be sensitive to penicillin after 10 years. Another is that drug side effects are sometimes labelled as allergic reactions. In other words, a common side effect such as nausea might be labeled an allergy instead. And if that happened to you in childhood, the likelihood is that you have no idea why you have the label "penicillin allergy" in your chart. You just know you've been told you should never be treated with penicillin.
Labels matter. A lot.
If you really have a severe allergy to penicillin, your healthcare providers have to be very careful c hoosing antibiotics. Antibiotics in the penicillin family are effective for a wide variety of infections. Some of the older ones are very useful for common illnesses, like ear infections, strep throat, mild skin infections, and others. One of their advantages is that they target a limited number of bacteria -- they are "narrow spectrum" antibiotics. Let's talk about why that's a good thing.
hoosing antibiotics. Antibiotics in the penicillin family are effective for a wide variety of infections. Some of the older ones are very useful for common illnesses, like ear infections, strep throat, mild skin infections, and others. One of their advantages is that they target a limited number of bacteria -- they are "narrow spectrum" antibiotics. Let's talk about why that's a good thing.
Antibiotics are designed to kill bacteria, or to help your own immune system kill bacteria. Some antibiotics, like penicillin, have a narrow spectrum, meaning that they only work for a limited number of bacteria. But the more infections are treated with penicillin, the more those bacteria find ways around it. New antibiotics must be developed to work on "resistant" bacteria. Many of the new antibiotics work for the original bacteria, too. They're called "broad spectrum" antibiotics because they work for many different bacteria.
That sounds like a good thing, right? The problem is that the more those broad spectrum antibiotics are used, the more bacteria find ways around them, too. So now we have more infections that are much harder to treat. And that happens not only in the general population, it happens in individuals like you and me. If our bodies are exposed to broad spectrum antibiotics over and over, we're more likely to end up with infections that are hard to treat.
"Penicillin allergy" tells your doctor that it's too dangerous to use any drug in the penicillin class,. There's often concern that drugs related to penicillin might be too dangerous, too. In that case, drugs that aren't related to penicillin are safer, and most often they are broad spectrum..
If you truly have a penicillin allergy, having broad spectrum drugs available is a wonderful thing. You can get effective treatment for infections without the concern of a life-threatening allergic reaction. But if you're one of the many who aren't really allergic to penicillin, you may be needlessly exposed to broad-spectrum antibiotics during your lifetime. And down the line you may end up having more infections that are harder and harder to treat. If that's not enough, the cost of those newer, broad spectrum antibiotics is typically much higher than older drugs like penicillin.
So what do you do if you aren't sure the label of "penicillin-allergic" is really true for you?
If you still have access to medical records from the time you were labelled "penicillin-allergic", track them down and find out what exactly happened. That can shed a lot of light on whether you should have that label or not.
If your old records aren't available, consider talking with your d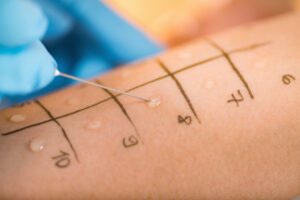 octor about allergy testing. A common method is the skin test, where a tiny amount of the possible allergen is introduced into the skin. If that results in a good-sized bump (or "wheal"), allergy is confirmed. If not, there is no allergy. Undergoing skin testing can tell you once and for all if you are truly allergic to penicillin. This type of testing is done at some doctor's offices, and if you're curious about the procedure we can explore it in more detail in another post.
octor about allergy testing. A common method is the skin test, where a tiny amount of the possible allergen is introduced into the skin. If that results in a good-sized bump (or "wheal"), allergy is confirmed. If not, there is no allergy. Undergoing skin testing can tell you once and for all if you are truly allergic to penicillin. This type of testing is done at some doctor's offices, and if you're curious about the procedure we can explore it in more detail in another post.
Find out if the label of "penicillin allergy" is really true for you!
One more way to take charge of your health is to make sure your allergy list correct. And that's what Better My Meds strives to do - help you take charge of your health! If you have any questions about this subject (or any other) please use the comment section below this post. Or contact us directly at Better My meds - we love hearing from you!
This is a test.
![]()